The saga of the UnitedHealth Care CEO assassination has, as might be anticipated, now became a dialogue of our well being care system. Elizabeth Warren, as an illustration, is making the apparent level that individuals hate the well being care system.
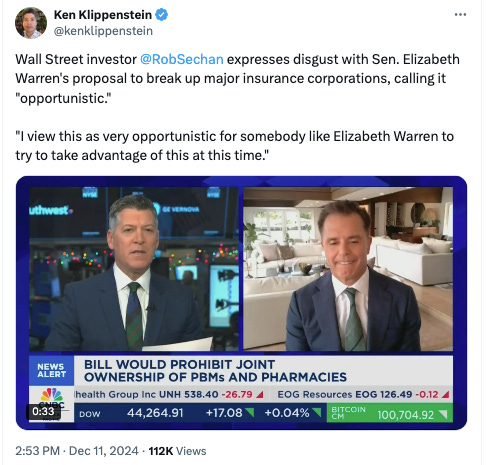
Then, productively, she proposed, together with Republican Senator Josh Hawley, laws to separate aside a few of these monster corporations from their pharmacy subsidiaries, thus decreasing conflicts of curiosity in well being care. While this laws was within the works lengthy earlier than the killing, it didn’t cease Wall Street buyers from saying that any dialogue of well being care reform was a de facto endorsement of homicide.
These sorts of discussions are all the time accomplished in dangerous religion, since individuals who make some huge cash from killing folks with spreadsheets prefer to fake to be very offended when anybody factors out well being care is a matter of life and demise. That stated, ethical hypocrisy isn’t the first cause our well being care system is so problematic. A extra necessary objection to reform is from a sure dominant pressure of pondering amongst economists and well being care wonks, who query whether or not the well being insurers are actually that dangerous. Economics blogger Noah Smith epitomized this view when he wrote a chunk titled “Insurance corporations aren’t the primary villain of the U.S. well being system.”
Anger at insurers displays, in his phrase, “deep-seated widespread misconceptions in regards to the U.S. well being care business. A complete lot of individuals — perhaps even most folks — appear to treat medical health insurance corporations as the primary villains within the system, when in reality they’re solely a really minor supply of the issues.” In different phrases, insurers are hated not as a result of they do dangerous issues, however as a result of they do one thing that’s needed: rationing.
In reality, he says, the precise villains are the folks taking good care of you, the “smiling physician” who is aware of the value however received’t let you know upfront. “So you get to hate UnitedHealthcare and Cigna,” Smith says, “whereas the true folks taking away your life’s financial savings and placing you liable to chapter get to play Mother Theresa.” These medical doctors and nurses rent insurers for a modest charge in return for showing just like the dangerous man, whereas the caregivers giggle all the way in which to the financial institution.
Smith sees this false impression as borne of our expertise with the system. Doctors, nurses, technicians – what he problematically lumps along with a broader class of company “suppliers” – care for us, so we like them, whereas insurers are simply paper pushers, and so we react negatively. Yet it’s the “suppliers,” Smith notes, who generate a lot of the waste and revenue. Insurers, against this, maintain down these prices. Anger at UnitedHealth Group is only a large misunderstanding. The true villain, he says, is the physician. (Eric Levitz of Vox, which because it seems is financed by the medical health insurance business, additionally argued that grasping medical doctors are the true downside, as does Biden supporter and pundit Matt Yglesias.)
To assist this view, Smith makes a few factors. First, he argues insurance coverage simply isn’t very worthwhile. UnitedHealth Group has a revenue margin of six %, which is half of the margin of regular public corporations. The firm makes some huge cash, with a web earnings of $23 billion in 2023, however that’s small in comparison with the $371 billion in general income, $241.9 billion of which, he says, is paid out in medical prices. Second, out of pocket bills are decrease percentage-wise than what folks in different international locations expertise. He places this chart up. We don’t pay extra extra out of pocket percentage-wide, it’s simply the extent of value is much too excessive, due to ‘suppliers.’
Matt Bruenig does an glorious job of exhibiting why Smith’s numbers are off (although his ‘single payer or bust’ framework is pointless, as there are a lot of nations with out single payer who nonetheless have a lot decrease waste). One apparent downside with Smith’s evaluation is that accounting income are a dumb option to perceive surplus spending. A much better means is simply to take a look at administrative bloat. In 2020, one examine confirmed that 34% of American expenditures on well being care was spent on administration, about $2497 per capita, versus $551 in Canada. There are loads of different research illustrating excessive administrative burdens.
That stated, administrative bloat and extra income, although large, understate the issue, as a result of even the place there technically isn’t waste, American drugs, in keeping with medical doctors, is getting much more bureaucratic. I need to concentrate on among the historical past of well being care reform, and clarify the conceptual flaws on the coronary heart Smith’s views, as a result of they aren’t some remoted fringe perspective. His formulation of the issue in well being care–who is accountable, and the way we should always repair it– are broadly held throughout the political aisle amongst well being coverage sorts and economists who’ve designed our well being system of the final variety of a long time, together with Obamacare.
Everyone agrees on the essential downside with U.S. well being care, which is that we spend an excessive amount of and have poor outcomes. The disagreement is about why. Smith thinks the guts of the well being care downside is that Americans over-consume, resulting from “ethical hazard.” We get a tax-break to purchase medical health insurance, which we pay in premiums, however we don’t pay on the counter when really getting companies. It’s like paying upfront for an all-you-can-eat buffet, you then have an incentive to take as a lot care as potential. And medical doctors have an incentivize to over-order it as a result of they’re paid below the much-maligned “charge for service” mannequin. In that mannequin, clinicans have been paid per service–an workplace go to, a x-ray, a process. But that led, within the “over-consumption” mind-set, to waste.
Economists, seeing this ethical hazard, sought to repair it with high-deductible plans, designed so we’d have “pores and skin within the recreation” and should pay every time we need to eat a service that we already purchased by means of premiums. But it wasn’t simply sufferers who wanted pores and skin within the game–the clinicians, particularly medical doctors, additionally wanted pores and skin within the recreation to appropriate the misaligned incentives of fee-for-service.
This principle of overconsumption dates again a long time, most notably to the rise of “managed care” within the 1970 and 80s. To comprise over-utilization by means of the non-public sector, the thought was to empower insurance coverage corporations by means of the rise of well being upkeep organizations, or HMOs. These organizations would pursue enterprise ways that prohibit how a lot sufferers use the well being care system; this was and remains to be known as “utilization administration.”
These practices included “community design,” or what we all know as having medical doctors out of our community, so we are able to’t see them. They additionally included “profit design,” which is what I describe above: excessive copays and deductibles so we use much less care. Then there have been the mechanisms to regulate medical doctors, prior authorization being the massive one. The different was often called “capitation” or “danger bearing.” The concept was to have physicians assume the operate of an insurance coverage firm. Instead of paying per service, insurance coverage corporations would give doctor teams or a hospitals a lump sum funds, hoping physicians would higher handle utilization as a result of they may flip a revenue by minimizing companies delivered. Managed care spurred a wave of hospital and doctor consolidation within the 90s, and prompted large backlash from clinicians and sufferers, who have been towards this kind of rationing from insurance coverage corporations.
Despite this backlash, as Hayden Rooke-Ley describes it, policymakers would double down on managed care in our public packages, Medicare and Medicaid. The concept, once more, was to interrupt from the fee-for-service mannequin. The Bush Administration in 2003 was the primary to make a significant transfer on this path by attempting to broaden the privatized model of Medicare, which he renamed to “Medicare Advantage.” As Rooke-Ley tells it, was an try to import HMOs into Medicare. The authorities would pay for care as a basket of companies in a single lump sum for a affected person. Instead of the fee-for-service mannequin, the place Medicare would pay physicians for every service, Medicare would pay a non-public insurance coverage firm to handle the prices of sufferers. What the insurere didn’t spend on care, they stored as revenue. Two a long time later, this is able to turn out to be a $500 billion greenback Medicare Advantage program, through which the federal government cuts a test of greater than $100B yearly to United Healthcare.
As Rooke-Ley describes, when the Democrats took over in 2008, they might embrace the speculation of managed care, however they might implement it in a different way, and name it by a brand new title: value-based care. And that will get to why Obamacare, aka the “Affordable Care Act,” was designed the way in which it was. The “overconsumption” thesis was put ahead in one of the influential articles in American well being care historical past, Atul Gawande‘s 2009 piece in The New Yorker titled “The Cost Conundrum” that articulated the rationale behind the ACA. In it, Gawande argued that Americans spend an excessive amount of on well being care as a result of medical doctors over-order it. “The most costly piece of medical gear, because the saying goes, is a health care provider’s pen,” he wrote. It is the “accumulation of particular person selections medical doctors make” that drive well being care prices. “And, as a rule, hospital executives don’t personal the pen caps. Doctors do.”
The apparent option to repair this dynamic can be to publicly ration care. Another means to do that can be to broaden the present system of personal rationing by means of insurance coverage corporations, ie commonplace managed care. But policymakers have been cautious of the backlash to managed care and burned from the Nineties-era battles over so-called HillaryCare, which successfully sought to place everybody in a managed care HMO and have these insurers compete by means of “managed competitors.” They wanted a distinct means of personal rationing of utilization. So they wanted to conceal the rationing. And that’s what they did. In 2009, as an illustration, economist Doug Elmendorf, a significant participant in coverage debates, testified to Congress as to the rationale well being care prices have been so overwhelming in America. He stated it explicitly.
Given the central position of medical expertise within the development of well being care spending, decreasing or slowing that spending over the long run will most likely require reducing the tempo of adopting new therapies and procedures or limiting the breadth of their software. Such adjustments needn’t contain express rationing however might happen because of market mechanisms or coverage adjustments that have an effect on the incentives to develop and undertake extra pricey therapies.
Elmendorf makes two claims right here. The first is that well being care spending is going on due to over-consumption of well being care therapies, largely primarily based on analysis within the 2000s from the Dartmouth Atlas of Health Care exhibiting that there was tons of of billions of {dollars} of waste within the system to chop out –the identical ones that Gawande relied on in his thesis.. The second is that to deal with this downside, it’s essential to ration, however not explicitly ration. You should do it by means of “market mechanisms.” Now, I’ll depart apart that Americans may be indignant about being misled by passive aggressive policymaking, even when they didn’t know precisely how, and simply level out that the purpose of Obamacare was not simply to broaden insurance coverage to the uninsured, however to extra assertively ration care for many who already had it. (And sure, there’s most likely a joke in right here about capitalism good communism dangerous.)
The outcome, as I discussed, was the enlargement of value-based care, the brand new title for the reimbursement mechanism that market-obsessed champions of the 80s and 90s sought to advertise. The concept was to appropriate the dangerous incentives of physicians by paying them not per service, however as a substitute having them assume the insurance coverage operate. If medical doctors might restrict how a lot sufferers used the well being care system, and resist their very own grasping impulses to supply an excessive amount of care, then they may revenue. This is what Elmendorf meant by “market mechanism.” Though this kind of contracting had receded with the backlash to managed care, it was occurring within the rising Medicare Advantage market. With the enlargement of value-based care, the thought was to rework all of well being care towards this kind of fee mannequin, beginning with common Medicare, which remained the most important “payer” of healthcare companies nationally.
And value-based care had a logic to it. The Republican-led managed care principle handled the “ethical hazard” of sufferers by empowering insurance coverage corporations to limit care choices and make sufferers put extra pores and skin within the recreation. To cope with the ethical hazard of physicians, we wanted to switch among the insurance coverage function–that pores and skin within the game–to them. With the correct financial incentives, they might ration whole use of case, driving down prices. What this meant in actuality was hospitals, non-public fairness, and insurance coverage conglomerates can be empowered to regulate physicians and different clinicians, as a result of medical doctors couldn’t assume this insurance coverage operate on their very own. Indeed 80 % of medical doctors at the moment are employed by certainly one of these company entities. UHG will not be solely the most important insurer, it’s the largest employer of physicians. And it’s the foremost champion of doing value-based care, which certainly one of its executives not too long ago described as as the brand new period of drugs is which physicians are now not in cost. That’s what all of those managed care reforms have amounted to, methods of placing friction between the affected person and drugs.
This all appeared cheap, as a result of care was too reasonably priced for sufferers, in order that they overused it, and physicians acquired paid for every service, in order that they delivered an excessive amount of of it.
This view wasn’t dangerous religion. Obama actually believed Gawande, the Dartmouth work, and all of the individuals who stated that there’s simply quite a lot of waste that needs to be simple to chop. That’s why he promised that you might preserve your physician, and that households would see decrease premiums by a median of $2500. But right here’s the factor. None of it labored to gradual the price of care. The “Affordable Care Act” didn’t make well being care reasonably priced, you couldn’t all the time preserve your physician, and prices stored going up. What occurred?
It seems the rationale well being care prices stored going up regardless of the reforms meant to reverse the trendline is as a result of policymakers misdiagnosed the underlying downside. The Dartmouth work was simply flawed on overuse of drugs. Higher medical prices in America have been results of, you guessed it, monopoly energy.
In 2003, 4 students printed a well-known article titled It’s the Prices, Stupid, discovering the U.S. pays extra and consumes much less on well being care than peer international locations. Though we spend twice as a lot, the U.S. has fewer medical doctors per capita, fewer hospital beds per capita, and among the many shortest hospital stays than different wealthy nations. We simply pay extra for what we get. These students reran the examine in 2019, after numerous reforms, and located the issue was the identical. Embedded within the costs for companies, as Breunig notes, are staggering administrative prices.
It wasn’t simply that policymakers essentially misdiagnosed our well being care downside. They additionally made one other grievous error, and that was the way in which they considered doing rationing. They didn’t say “we’re going to have a board of medical doctors make selections about what care can occur for what illness and what this can value,” which might be a public utility mannequin. Instead, managed care meant non-public rationing by means of consolidation.
They took hospitals, insurers, pharmaceutical middlemen, and physician’s practices, and put them below the thumb of financiers by means of waves of acquisitions. Putting hard-hearted bankers in cost, and saying you get to earn cash if you happen to cut back waste, was a seemingly merciless however needed method to the issue. Indeed, if you happen to discover a sure meanness to Smith’s argument, the type of informal cruelty we so usually see with establishment defending thinkers, that’s the place it comes from. You need me on that wall, you want me on that wall, or grandma’s gonna get an costly coronary heart surgical procedure that received’t assist her however that each one of us must pay for.
The outcome was waves of consolidation in each side of the system, from hospitals to drug shops to emergency room doctor companies. In February of 2020, I did a detailed evaluation of the rise of CVS, exhibiting that over a collection of mergers, the agency rolled up pharmacies, pharmaceutical middlemen, pressing care clinics, and insurers. UnitedHealth Group, between 2021-2023 alone, gained management over 1,300 new corporations. Now, anybody who is aware of something about monopolies can let you know instantly what would occur when an business will get consolidated. Prices go up, output goes down, and high quality will get worse. And that’s what occurred.
Yes, there are vital income all through the well being care system, however the true means that the monopolization exhibits itself is thru administrative overhead. Medicare Advantage, with its fancy capitation by means of monopolists like UnitedHealth Group, requires greater than $100 billion a 12 months extra than simply common Medicare in overpayments. That’s some huge cash. But this sort of waste is all over the place; the highest three pharmacy profit managers in America, who’re principally simply corporations who handle spreadsheets, have extra income than France spends on well being care.
The level is that it’s not “smiling medical doctors” who need to cost excessive costs for a hospital go to inflicting our downside; as I discussed, these medical doctors are largely simply workers now, working for an insurance coverage firm or a hospital or a non-public fairness agency. And that is illustrates the error when Smith refers to “suppliers” because the medical doctors and nurses., With company consolidation on each the supplier and insurance coverage aspect, what outcomes is huge administrative overhead and value gouging, a pink queen’s race the place each large firm is investing in administrative bloat to battle with each different large firm, usually with perverse spending outcomes that result in loopy quantities of waste in some areas and a complete lack of care in others. And the concept that medical doctors know what a value of an operation or process may be implies that there’s a single value. But there isn’t. A drug or process for one affected person might be 5 occasions as costly for another person, relying on their plan or different components.
And that will get to the ultimate conceptual downside. Smith may argue, effectively, certain there’s waste, however most of that isn’t within the medical health insurance sector, it’s in different areas of the well being enterprise. But that’s an outdated mind-set. Over the previous twenty years, we have now smooshed collectively strains of enterprise in well being care such that there isn’t a such factor as a pure “well being insurer” anymore. As I famous, United is the most important doctor employer and the nation’s chief in value-based care. It’s like calling Google an e mail firm. Sure it owns and runs Gmail, nevertheless it’s far more than that.
To perceive why this view doesn’t make sense, it helps to start out with some antitrust instances. The Biden Antitrust Division’s first merger problem was UHG shopping for fee community Change Health in an $8 billion greenback deal. As I famous, that merger was a disaster; a 12 months after the DOJ misplaced and the deal closed, Change acquired hacked and hospitals, medical doctors, and pharmacists misplaced entry to money circulate, permitting UHG to purchase up among the suppliers it had crippled.
But that’s not the one problem. In mid-November, the Antitrust Division sued UHG over its $3.3 billion greenback tried acquisition of house well being care and hospice supplier Amedisys. So the primary and final merger instances by Biden have been each towards UHG. And that’s not all, the Federal Trade Commission additionally sued UHG over its manipulation of drug pricing by means of its pharmacy profit supervisor arm. Here’s a report launched simply earlier than the lawsuit exhibiting what these PBM subsidiaries did, in keeping with one high-level government.
“We’ve created plan designs to aggressively steer prospects to house supply the place the drug value is ~200 occasions greater,” he wrote. If you went to Costco, he went on to say, the price was $97, so the plan didn’t suggest sufferers go there. If a affected person went to Walgreens, which the plan did suggest, it was $9000. And if a affected person selected house supply by way of the PBMs personal mail order pharmacy, it was $19,200. “The optics usually are not good and have to be addressed,” he added. He didn’t must say that the added income for PBMs, only for that one drug, was $902.1 million over a couple of years.
So UHG has been below quite a lot of authorized warmth. But discover one thing about these lawsuits? None of them should do with medical health insurance. UHG was sued over its manipulation of drug pricing, for getting a monetary firm, and for attempting to accumulate a bunch of medical caregivers.
UHG, in different phrases, will not be primarily a well being insurer, however one thing new. It is the most important employer of medical doctors within the nation, it has a big software program enterprise, and it sits in the midst of the pharmaceutical pricing chain with its OptumRx pharmacy profit supervisor and large mail-order pharmacy. In 2020, when the U.S. authorities delivered tens of billions of {dollars} to hospitals, guess what monetary conduit it used? Optum Bank, which can be owned by UHG. And it’s now within the pharmaceutical manufacturing enterprise, as is CVS.
UnitedHealth Group isn’t, as Noah Smith believes, spending $241.9 billion paying for medical prices, it’s attempting to determine use that cash from UnitedHealth Care – its insurance coverage arm – to purchase from Optum – its arm of all the pieces else. UHG even has a time period for this spending, ‘intercompany eliminations,’ which have now reached 27% of its income.
The knowledge exhibits that UnitedHealth’s inter-subsidiary enterprise dealings have been rising as a share of its whole income over time, virtually doubling over 16 years from about 15% in 2008. This signifies that UnitedHealthcare insurance coverage usually are not solely more and more paying to make use of Optum’s physicians, PBM, claims integrity processing and income cycle administration, however that UnitedHealth’s general development seems to be depending on these sorts of inner transactions.
A variety of what UnitedHealth Group is doing with the cash that Smith thinks is paying for well being care is just self-dealing.
This mannequin is new. In the 2000s, we used to have well being insurers, pharmacy profit managers, pharmaceutical corporations, hospitals, physician’s practices, software program corporations, and fee networks, and so they have been all unbiased and traded with each other as want be. There have been a couple of exceptions – Kaiser was each an insurer and hospital community, however for probably the most half, a well being insurer made cash promoting medical health insurance, a health care provider made cash promoting his companies, et al. Today, we have now UnitedHealth Group and CVS, which are attempting to take a chunk in each a part of the well being enterprise.
The mashing collectively of well being strains of enterprise is one thing prompted by the Bush-era adjustments in Medicare within the early 2000s, after which the creation of Obamacare, which, along with the value-based care reforms, capped income for insurers however nonetheless allowed these insurers to purchase suppliers. Because of this revenue cap, often called the “medical loss ratio,” insurers might solely make a sure sum of money by means of medical health insurance, however they may take their affected person cash and spend it on medical doctors they make use of utilizing software program they bought financed by a financial institution they owned. And now, they do. I wrote this up in a chunk about how Obamacare created large drugs.
A revenue cap just like the Medical Loss Ratio is usually an excellent factor for utility companies, however such rules have to be paired with a prohibition on increasing exterior of a easy line of enterprise. Otherwise, you get large conflicts of curiosity. And that’s the place economists, who suppose sure types of company consolidation are environment friendly and that conflicts of curiosity don’t a lot matter, got here into the image. FTC economists validated the smooshing collectively of sure strains of enterprise, seeing a pharmacy advantages supervisor proudly owning its personal mail order pharmacy, which UnitedHealth Group does, as useful, as a substitute of harmful.
Some policymakers have seen this enterprise mannequin shift. Last month, Antitrust AAG Jonathan Kanter gave a speech on the platformization of well being care, noting that we have now to cease enthusiastic about well being care giants as insurers, suppliers, PBMs, or medical doctors practices, or hospitals. They are, as he famous, the entire above. They are in some ways tech platforms, like Google proudly owning a search engine and steering folks to its different merchandise with that. These well being conglomerates have mimicked this technique. CVS in 2018 even known as itself a “uniquely highly effective platform,” bragging that it touched a 3rd of Americans with its drug retailer chain, Aetna insurance coverage firm, pressing care clinics, and PBM. Kanter known as the issue “well being care Tetris.”
And this dynamic isn’t only a operate of insurers shopping for up and down the worth chain. Everyone is smooshing collectively. In Pennsylvania, large hospital techniques are taking up the insurance coverage business, drug distributors are shopping for oncology clinics, and even Kaiser – maybe the one built-in system that really delivers actual built-in care – is increasing right into a extra assertive financialized mannequin. Here’s an inventory of the highest twenty companies in America by income. Seven are well being conglomerates, all of which have many various strains of enterprise.
It’s a lot worse than only one insurance coverage firm integrating into an octopus, all elements of the system are being systematically corrupted by conflicts of curiosity. For occasion, take an instance I heard not too long ago. Oncologists at smaller practices are prepared to strive actually new medication as a result of they know the analysis and know it’s the greatest drug for the affected person’s illness. But oncologists at practices owned by large distributors are sometimes robotic and compliant, prescribing from an inventory of medicine, often called a ‘formulary,’ handed down from their employer, medication which might be extra prone to earn cash for the distributor dad or mum. To get to the ideological level, such formularies are express rationing mechanisms, and the Pharmacy and Therapeutics committees that design them are successfully demise panels (although they’d by no means consider themselves in that gentle).
But even placing apart the conflicts, value-based care itself will increase administrative prices by an infinite margin. There are total industries dedicated to developing with metrics (NQF, PQA, and so on), there’s a ton of coding inside digital well being data to have the ability to measure these metrics (which creates a well being document monopoly known as Epic Systems), and there’s employees inside hospitals and clinics and insurers to trace all the pieces. Value primarily based care’s administrative complexity additionally makes it unimaginable to have a small apply, you need to be half of a big sufficient group that the measurements may be statistically significant, so that you get “clinically built-in networks” of larger physician practices. As one particular person advised me:
The period of time I’ve personally noticed folks (together with clinicians and directors) spending on VBC stuff is insane. It consumes SO a lot time and effort- it may be significant; it won’t be, nevertheless it positively contributes to administrative overhead.
Add to that the truth that we dwell in a multi-payer system the place each single payer has totally different metrics they need to concentrate on in your bonus, and the admin turns into thoughts bogglingly big. UHC desires you to work on readmissions, Aetna desires you to work on hospital acquired infections, Cigna desires you to work on getting folks to get their prescriptions in 100 day provides, and Centene desires you to get the entire folks with bronchial asthma to have an motion plan.
In different phrases, we have now giant unmanageable bureaucratic nightmare companies negotiating with one another throughout countless strains of enterprise, together with un-trackable flows of cash and opaque pricing. These companies in flip create a kind of cartel of giants, the way in which Google and Apple reduce a deal to separate search income. That’s why Americans really feel like we’re a weird monetary system the place care is sort of incidental, and clinicians and sufferers are annoyed.
Ultimately, as Rooke-Ley observes, the options are fairly easy. Policymakers must cease micromanaging clinicians and sufferers in pursuit of much less use of well being care, and transfer energy again to clinicians and their sufferers, and out of the fingers of bankers. We should see well being care as public infrastructure. We already see the world this manner; emergency rooms should take all comers. And 70% of healthcare is already financed by means of the federal government, which is greater than every other nation spends.
It’s not that revenue is dangerous, or that we’d like a selected type of public or non-public fee. Any mannequin can work. But we have now to remove bargaining energy and conflicts of curiosity as the important thing strategic targets amongst well being care executives; that’s the premise of the Hawley/Warren invoice to separate off pharmacies from the remainder of the well being conglomerate. Let’s go additional and do it throughout the board, forcing corporations to divest strains of enterprise that create conflicts of curiosity. We additionally want publicly accessible, clear costs the place folks pay the identical value for a similar good or service, as Indiana Republican Senator Jim Banks suggests for hospitals. If we are able to put these incentives in place, then quite a lot of these corporations will break up themselves aside, because it received’t be price it to be a big inefficient conglomerate.
We additionally should re-conceptualize the thought of the well being care “enterprise.” The quantity of monetary bullshit on this a part of the economic system is insane, and pretend entrepreneurs are always spreadsheet jockeying for cash. So on a fundamental degree, if you happen to’re not producing drugs or coping with sufferers, you need to most likely be employed by the federal government or in an administrative position making very skinny revenue margins. These are lives we’re speaking about.
To conclude, Smith’s argument is flawed, however extra importantly misses the purpose. The public isn’t flawed to hate these large conglomerates. These are the corporations which have energy of life and demise over us. And there are a lot of causes to see UnitedHealth Group as a very noxious company, as a result of it reaches into each a part of the well being enterprise, and has lobbying and political energy designed to thwart a public-minded system. But in the end, it’s not simply UHG. In reality, UHG’s existence is a results of sloppy pondering amongst well being coverage wonks and economics-minded individuals who haven’t adopted the business. And we ought to start out by correcting that.
Thanks for studying. Send me recommendations on bizarre monopolies, tales I’ve missed, or feedback by clicking on the title of this article. Or if you happen to work for or adjoining to a monopoly and have attention-grabbing confidential stuff to share, go forward and try this. If you appreciated this problem of BIG, you possibly can enroll right here for extra problems with BIG, a publication on restore truthful commerce, innovation and democracy. If you actually appreciated it, learn my ebook, Goliath: The 100-Year War Between Monopoly Power and Democracy.
cheers,
Matt Stoller